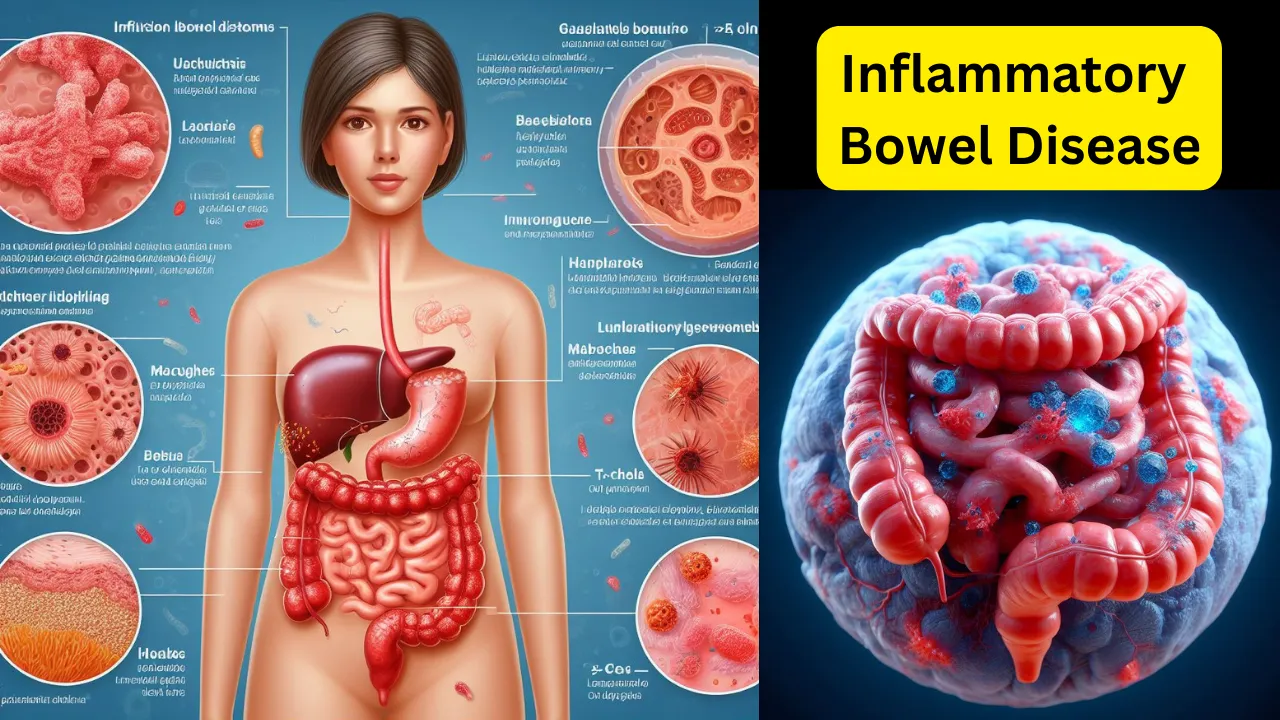
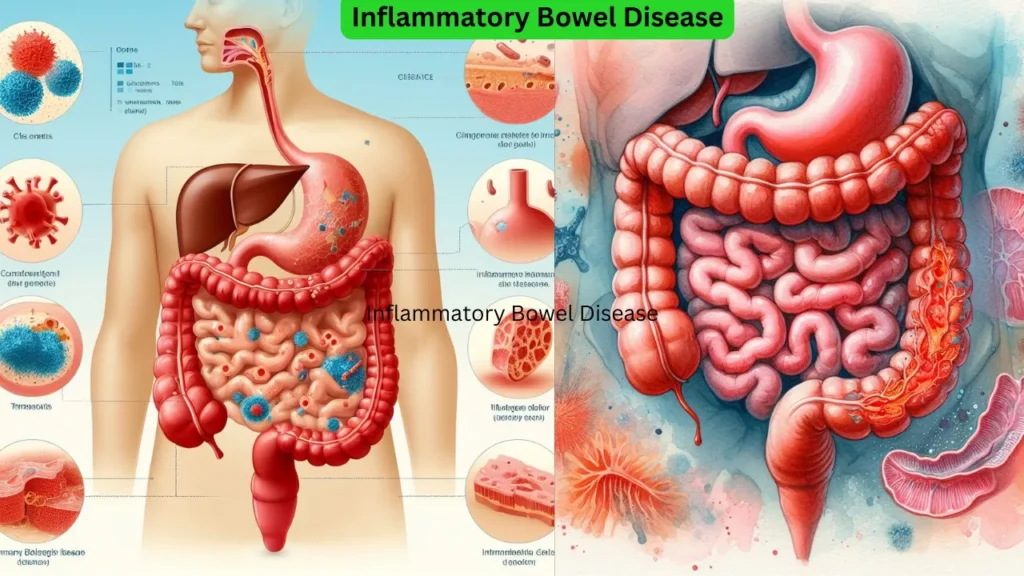
Inflammatory Bowel Disease (IBD) is a term used to describe chronic inflammation of the digestive tract. The two primary types of IBD are Crohn’s disease and Ulcerative Colitis. These conditions can cause significant discomfort and often require lifelong treatment or management.
I. Introduction
Inflammatory Bowel Disease (IBD) refers to chronic inflammation of the digestive tract. It encompasses two main types: Crohn’s disease and Ulcerative Colitis. Both conditions can lead to severe discomfort and require ongoing treatment. The impact of IBD on individuals is substantial, with approximately 1.6 million Americans currently affected and an additional 70,000 new cases diagnosed each year. This not only takes a physical toll but also affects individuals emotionally and socially.
II. Types of Inflammatory Bowel Disease
A. Crohn’s Disease
Crohn’s disease is a type of IBD that can affect any part of the digestive tract, although it most commonly impacts the small intestine or the colon. Symptoms of Crohn’s disease often include abdominal pain, diarrhea, weight loss, and malnutrition.
Diagnosing Crohn’s disease typically involves a combination of blood tests, stool tests, imaging tests, and endoscopic procedures. Treatment options for Crohn’s disease vary but may include medication, nutritional therapy, and in severe cases, surgery. It’s important to note that the long-term effects of Crohn’s disease can include intestinal obstruction, fistulas (abnormal connections between organs), and malnutrition.
B. Ulcerative Colitis
Ulcerative colitis primarily affects the colon and rectum. Common symptoms of this condition include abdominal pain, bloody diarrhea, and a constant urge to defecate.
The diagnosis of Ulcerative colitis often involves a colonoscopy and sample tissue biopsy. Treatment usually revolves around medication to reduce inflammation and control symptoms. However, in severe cases, surgical intervention may be necessary. It’s worth noting that potential long-term effects of Ulcerative colitis include an increased risk of colon cancer and liver disease.
III. Causes and Risk Factors
The exact cause of IBD remains unknown, but research suggests that several factors may contribute to its development.
A. Genetic factors
Genetics play a significant role in the development of IBD. Individuals with a family history of the disease have a higher risk of developing it themselves. Certain genetic mutations have also been identified as potential risk factors for IBD.
B. Environmental triggers
Environmental factors can also influence the development or exacerbation of IBD. Dietary choices, smoking habits, and exposure to certain infections may contribute to the onset or progression of the disease.
C. Immune system dysfunction
A dysfunctional immune system is believed to be a key factor in the development of IBD. In this condition, the body’s immune response mistakenly attacks healthy cells in the digestive tract, leading to chronic inflammation.
D. Microbiome imbalance
Emerging research suggests that an imbalance in the gut microbiome, the collection of microorganisms residing in the digestive tract, may contribute to the development of IBD. Disruptions in the delicate balance of beneficial and harmful bacteria can trigger inflammation and contribute to the progression of the disease.
In conclusion, Inflammatory Bowel Disease (IBD) encompasses conditions such as Crohn’s disease and Ulcerative Colitis, which cause chronic inflammation in the digestive tract. The exact cause of IBD remains unclear, but factors such as genetics, environmental triggers, immune system dysfunction, and microbiome imbalance are thought to contribute to its development. It’s crucial for individuals with IBD to work closely with healthcare professionals to manage their condition effectively and improve their quality of life.
IV. Symptoms of Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a chronic condition that affects the gastrointestinal tract. It is characterized by inflammation and damage to the lining of the digestive system. There are two main types of IBD: Crohn’s disease and ulcerative colitis. Both conditions can cause a range of symptoms that can vary in severity from person to person. In this article, we will explore the common symptoms associated with Inflammatory Bowel Disease.
1. Abdominal Pain and Cramping
One of the primary symptoms of Inflammatory Bowel Disease is abdominal pain and cramping. This discomfort often occurs in the lower abdomen and may be severe. It can come and go or persist for extended periods. The pain is caused by inflammation and ulcers in the intestinal lining, which can lead to spasms and discomfort.
Possible causes of abdominal pain and cramping in IBD:
- Inflammation and ulcers in the intestinal lining can irritate the nerves in the abdomen, leading to pain and cramping.
- The immune system’s response to the inflammation can cause the release of chemicals that trigger pain signals.
- Obstruction or narrowing of the intestines due to scarring or inflammation can result in cramping pain.
Ways to manage abdominal pain and cramping:
- Taking prescribed medications such as anti-inflammatory drugs, pain relievers, or antispasmodics can help alleviate abdominal pain and cramping.
- Applying heat to the abdomen or taking warm baths may provide temporary relief.
- Practicing stress-reducing techniques like deep breathing, meditation, or yoga can help relax the muscles and reduce pain.
2. Diarrhea
Frequent diarrhea is another hallmark symptom of Inflammatory Bowel Disease. The stools may be loose, watery, and may contain blood or mucus. Diarrhea occurs due to the inflammation and ulceration in the digestive tract, which disrupts the normal absorption of water and nutrients. This can lead to increased urgency and frequency of bowel movements.
Factors contributing to diarrhea in IBD:
- Inflammation and ulcers in the intestines can impair the absorption of water, resulting in loose stools.
- Increased secretion of fluids into the intestines due to inflammation can also contribute to diarrhea.
- Bacterial overgrowth or infections in the gut can worsen diarrhea symptoms.
Tips for managing diarrhea:
- Stay hydrated by drinking plenty of fluids to replace the lost water and electrolytes from diarrhea.
- Avoid foods that can exacerbate diarrhea, such as spicy or greasy foods, caffeine, and alcohol.
- Incorporate fiber-rich foods gradually into the diet to help regulate bowel movements. However, consult with a healthcare professional or a registered dietitian for personalized dietary recommendations.
3. Rectal Bleeding
Rectal bleeding is a common symptom of ulcerative colitis, a type of Inflammatory Bowel Disease that primarily affects the colon and rectum. The inflammation and ulcers in the rectum can cause bleeding, which may be seen in the stool or on toilet paper. It is essential to consult a healthcare professional if rectal bleeding occurs, as it can indicate more severe complications.
Possible causes of rectal bleeding in IBD:
- Inflammation and ulceration in the rectum can lead to the rupture of small blood vessels, resulting in rectal bleeding.
- Chronic inflammation can cause thinning of the intestinal lining, making it more susceptible to bleeding.
Management strategies for rectal bleeding:
- Topical medications, such as corticosteroid suppositories, can help reduce inflammation and promote healing of the rectal ulcers.
- Maintaining good hygiene by using gentle, unscented toilet paper and avoiding excessive wiping can prevent further irritation and bleeding.
- If rectal bleeding is severe or persistent, medical intervention may be necessary, including the use of oral medications or surgical interventions.
4. Weight Loss and Malnutrition
Inflammatory Bowel Disease can interfere with the absorption and digestion of nutrients, leading to weight loss and malnutrition. The chronic inflammation in the digestive tract increases the body’s energy expenditure, making it difficult to maintain a healthy weight. Additionally, diarrhea and reduced appetite can further contribute to weight loss and nutrient deficiencies.
Factors contributing to weight loss and malnutrition in IBD:
- Malabsorption of nutrients due to inflammation and damage to the intestinal lining can lead to nutrient deficiencies and weight loss.
- Chronic inflammation can increase the metabolic rate, causing the body to burn more calories than it takes in.
- Loss of appetite, nausea, and dietary restrictions due to IBD symptoms can result in inadequate calorie and nutrient intake.
Strategies to address weight loss and malnutrition:
- Working with a registered dietitian can help develop an individualized meal plan that focuses on optimizing nutrient intake and managing symptoms.
- Incorporating nutrient-dense foods such as lean proteins, fruits, vegetables, and whole grains can help meet nutrient needs.
- In some cases, nutritional supplements or enteral nutrition (tube feeding) may be recommended to support weight gain and provide necessary nutrients.
5. Fatigue and Weakness
Chronic inflammation and malabsorption of essential nutrients can result in fatigue and weakness in individuals with Inflammatory Bowel Disease. The body’s constant immune response and the lack of proper nourishment can leave individuals feeling drained and low on energy. It is crucial to manage the condition effectively to minimize fatigue and improve overall well-being.
Causes of fatigue and weakness in IBD:
- Chronic inflammation triggers the release of pro-inflammatory cytokines, which can contribute to feelings of fatigue and weakness.
- Nutrient deficiencies, particularly iron and B-vitamins, can impact energy levels and lead to fatigue.
- Interrupted sleep patterns due to symptoms like pain and frequent bowel movements can also contribute to fatigue.
Tips for managing fatigue and weakness:
- Prioritize rest and sleep to allow the body to recover and recharge.
- Engage in regular physical activity, such as low-impact exercises, to improve energy levels and reduce fatigue.
- Ensure an adequate intake of nutrients through a well-balanced diet and consider supplements if deficiencies are identified.
6. Fever
Fever is a common symptom that can occur during flare-ups of Inflammatory Bowel Disease. It is often accompanied by other symptoms such as abdominal pain and diarrhea. The fever is a result of the body’s immune response to the inflammation in the digestive tract. Monitoring body temperature and seeking medical attention for persistent or high fever is important.
Reasons behind fever in IBD:
- The immune system’s response to inflammation can trigger the release of chemicals called pyrogens, which raise body temperature.
- Infection or complications related to IBD can also cause fever.
Approaches to managing fever:
- Over-the-counter antipyretic medications like acetaminophen can help reduce fever. However, consult with a healthcare professional before taking any medication.
- Resting, staying hydrated, and applying cool compresses can provide relief from fever symptoms.
- If fever persists or is accompanied by severe symptoms, medical evaluation is necessary to identify the underlying cause and appropriate treatment.
7. Loss of Appetite
Inflammatory Bowel Disease can lead to a loss of appetite, which can further contribute to weight loss and malnutrition. The inflammation in the digestive tract can cause feelings of fullness, nausea, and a lack of interest in food. It is essential to ensure adequate nutrition by working with a healthcare professional or a registered dietitian to develop a suitable diet plan.
Causes of loss of appetite in IBD:
- Inflammation in the digestive tract can affect the production of appetite-regulating hormones, leading to a decrease in appetite.
- Nausea, abdominal pain, and other gastrointestinal symptoms can make eating unpleasant and decrease appetite.
- Medications used to manage IBD, such as corticosteroids, can also affect appetite.
Strategies to address loss of appetite:
- Eating smaller, more frequent meals instead of large meals can help manage appetite and prevent feelings of fullness.
- Including foods that are easy to digest and well-tolerated, such as soups, smoothies, and cooked vegetables, can provide essential nutrients without overwhelming the gastrointestinal system.
- Experimenting with different flavors and textures, while being mindful of trigger foods, can make meals more appealing.
8. Joint Pain and Inflammation
Some individuals with Inflammatory Bowel Disease may experience joint pain and inflammation, a condition known as peripheral arthritis. The inflammation in the gut can trigger an immune response in other parts of the body, leading to joint pain and swelling. Seeking medical advice is important to manage joint symptoms effectively and minimize their impact on daily life.
Factors contributing to joint pain and inflammation in IBD:
- Inflammatory mediators released during the immune response in the gut can migrate to the joints and cause inflammation.
- Autoimmune mechanisms may play a role in joint involvement in IBD.
- Nutrient deficiencies, particularly vitamin D and calcium, can contribute to joint symptoms.
Approaches to managing joint pain and inflammation:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be prescribed to alleviate joint pain and reduce inflammation. However, NSAIDs should be used with caution, as they can exacerbate gastrointestinal symptoms in some individuals.
- Physical therapy and regular exercise, under the guidance of a healthcare professional, can help improve joint function and reduce pain.
- Ensuring adequate intake of nutrients involved in bone and joint health, such as calcium, vitamin D, and omega-3 fatty acids, may help manage joint symptoms.
9. Skin Disorders
Inflammatory Bowel Disease has been associated with various skin disorders. Conditions such as erythema nodosum and pyoderma gangrenosum can occur as a result of the inflammation in the body. These skin conditions are characterized by painful, red, and swollen bumps or ulcers. Proper management of the underlying IBD can help alleviate these skin manifestations.
Possible causes of skin disorders in IBD:
- Inflammatory mediators released during the immune response in IBD can affect the skin and cause various skin manifestations.
- Genetic factors and alterations in the immune system may contribute to the development of skin disorders.
Tips for managing skin disorders associated with IBD:
- Topical corticosteroids or other prescribed medications can help reduce inflammation and promote healing of skin lesions.
- Maintaining good skin hygiene and avoiding irritants can prevent further skin damage and complications.
- Close collaboration between dermatologists and gastroenterologists is important for comprehensive management of skin disorders in individuals with IBD.
10. Eye Inflammation
Eye inflammation, or uveitis, can occur in individuals with Inflammatory Bowel Disease. It is characterized by redness, pain, and blurred vision. Immediate medical attention is required as untreated uveitis can lead to serious complications and potentially affect vision. Coordinating care between gastroenterologists and ophthalmologists is crucial for optimal management.
Reasons behind eye inflammation in IBD:
- Inflammatory mediators in the body can affect the eyes and lead to inflammation.
- Autoimmune mechanisms may contribute to the development of uveitis in individuals with IBD.
Approaches to managing eye inflammation:
- Treatment of eye inflammation typically involves the use of corticosteroid eye drops or other medications prescribed by an ophthalmologist.
- Regular eye exams and close monitoring of eye symptoms are important to detect and manage uveitis promptly.
- Coordinated care between a gastroenterologist and an ophthalmologist ensures comprehensive management of eye inflammation in individuals with IBD.
In conclusion, Inflammatory Bowel Disease presents a range of symptoms that can significantly impact an individual’s quality of life. If you or someone you know experiences any of the mentioned symptoms, it is essential to seek medical advice for an accurate diagnosis and appropriate management. Early intervention and effective treatment can help alleviate symptoms, reduce inflammation, and improve overall well-being for those living with Inflammatory Bowel Disease.
V. Diagnosis and Diagnostic Tests for Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) encompasses a group of chronic conditions that result in inflammation within the digestive tract, including Crohn’s disease and ulcerative colitis. Accurate and timely diagnosis is crucial for effectively managing these diseases. In this article, we will delve into the various diagnostic tests and procedures used to diagnose IBD.
Medical History and Physical Examination
The diagnostic process for IBD typically commences with a comprehensive review of the patient’s medical history and a thorough physical examination. During the medical history review, the healthcare provider will inquire about symptoms such as persistent diarrhea, abdominal pain, weight loss, and rectal bleeding. Additionally, they will investigate whether there is any family history of IBD or other related conditions.
The physical examination involves palpating the abdomen to check for tenderness, swelling, or masses, and listening to bowel sounds. These initial steps aid the healthcare provider in assessing the patient’s overall health and determining the necessity for further testing.
Blood Tests
Blood tests are commonly employed to assist in the diagnosis of IBD. They provide valuable information about the patient’s general health and help rule out other conditions. Some of the blood tests used in diagnosing IBD include:
- Complete Blood Count (CBC): This test measures the levels of different blood cells, including red blood cells, white blood cells, and platelets. Abnormalities in these levels can indicate inflammation or anemia, which are common in IBD. A detailed analysis of the CBC can provide insights into disease severity and identify potential complications.
- C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR): These tests measure the levels of inflammation markers in the body. Elevated CRP or ESR levels suggest an ongoing inflammatory process, which is often observed in IBD. Monitoring these markers over time can help assess disease activity and response to treatment.
- Liver Function Tests: These tests evaluate the function of the liver and can help detect any liver abnormalities that may be associated with IBD. Liver function abnormalities can occur in some individuals with IBD, and assessing liver function is important for overall disease management.
Stool Tests
Stool tests are commonly performed to aid in the diagnosis of IBD and exclude other conditions that may manifest similar symptoms. These tests involve analyzing a sample of the patient’s stool for various markers, including:
- Calprotectin: This protein is released by white blood cells during inflammation. Elevated levels of calprotectin in the stool can indicate active inflammation in the digestive tract, suggesting the presence of IBD. Monitoring calprotectin levels can provide insights into disease activity and response to treatment.
- Stool Cultures: These tests help identify any infectious organisms that may be causing the symptoms, which is important for ruling out infectious causes of bowel inflammation. By analyzing the stool sample for the presence of specific bacteria or parasites, healthcare providers can ensure appropriate treatment and avoid unnecessary interventions.
Endoscopic Procedures
Endoscopic procedures play a crucial role in diagnosing IBD. They involve using a flexible tube with a camera (endoscope) to examine the digestive tract and obtain tissue samples (biopsies) for further analysis. Some commonly used endoscopic procedures for diagnosing IBD include:
- Colonoscopy: This procedure allows visualization and examination of the entire colon and the ileum, which is the last part of the small intestine. During a colonoscopy, the healthcare provider can identify areas of inflammation, ulcers, or other abnormalities. Biopsies can be taken during the procedure to confirm the diagnosis and differentiate between different types of IBD.
- Flexible Sigmoidoscopy: This procedure focuses on examining the rectum and lower part of the colon. It is particularly useful for evaluating the extent and severity of inflammation in ulcerative colitis. By visualizing the affected areas, healthcare providers can determine the appropriate treatment approach and monitor disease progression.
- Upper Endoscopy: Also known as esophagogastroduodenoscopy (EGD), this procedure involves examining the esophagus, stomach, and the first part of the small intestine (duodenum). It helps assess inflammation and identify any ulcers or other abnormalities in these areas. Upper endoscopy is especially relevant for diagnosing Crohn’s disease, as it can detect involvement of the upper digestive tract.
- Capsule Endoscopy: In this procedure, the patient swallows a small capsule containing a camera that takes pictures as it passes through the digestive tract. It provides a detailed view of the small intestine, which is otherwise challenging to visualize using other endoscopic procedures. Capsule endoscopy can be helpful in evaluating the extent and location of inflammation in Crohn’s disease.
Imaging Studies
Imaging studies can be instrumental in diagnosing and monitoring IBD. They provide detailed images of the digestive tract, enabling healthcare providers to identify structural changes and assess disease activity. Some common imaging techniques used in diagnosing IBD include:
- X-ray: Although not specific for IBD, an abdominal X-ray can help detect complications such as intestinal blockages or perforations. It is a useful initial screening tool in certain cases and may guide further diagnostic investigations.
- Computed Tomography (CT) Scan: This imaging technique combines X-rays with computer technology to create detailed cross-sectional images of the digestive tract. It can help assess the extent of inflammation, detect complications, and guide treatment decisions. CT scans are particularly valuable in evaluating disease behavior and identifying abscesses or strictures.
- Magnetic Resonance Imaging (MRI): MRI utilizes a magnetic field and radio waves to generate high-resolution images of the digestive tract. It is particularly useful for evaluating the small intestine and detecting complications such as abscesses or fistulas. MRI can provide valuable information about disease activity and response to therapy.
Genetic Testing
Genetic testing may be utilized in certain cases to help confirm the diagnosis of IBD and assess the risk of developing these conditions. It involves analyzing specific genes associated with IBD, such as the NOD2/CARD15 gene. However, it is important to note that genetic testing alone is not sufficient for diagnosing IBD, as many patients with IBD do not have these genetic mutations. Genetic testing can be valuable in certain clinical scenarios, such as when there is uncertainty about the diagnosis or when assessing disease risk in family members.
Conclusion
Diagnosing IBD requires a comprehensive approach that involves a thorough medical history review, physical examination, blood tests, stool tests, endoscopic procedures, imaging studies, and sometimes genetic testing. Each diagnostic test provides unique and valuable information that aids in confirming the diagnosis, evaluating disease activity, and guiding treatment decisions. If you suspect you may have IBD or are experiencing symptoms, it is crucial to consult a healthcare provider who can perform the necessary diagnostic tests and guide you through the treatment process.
VI. Coping with Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) refers to a group of chronic conditions that cause inflammation in the digestive tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. These conditions can have a significant impact on a person’s quality of life, but with the right coping strategies, individuals can manage their symptoms effectively. This article will provide valuable insights and tips on how to cope with Inflammatory Bowel Disease.
Understanding Inflammatory Bowel Disease
Before delving into coping strategies, it is essential to have a basic understanding of Inflammatory Bowel Disease. Both Crohn’s disease and ulcerative colitis involve chronic inflammation of the gastrointestinal tract, resulting in symptoms such as abdominal pain, diarrhea, fatigue, weight loss, and rectal bleeding. These symptoms can vary in severity and may come and go in flare-ups.
Inflammatory Bowel Disease is a complex condition that requires a comprehensive approach to management. It is crucial to work closely with a healthcare professional, preferably a gastroenterologist who specializes in digestive disorders. They can provide an accurate diagnosis, evaluate the severity of your condition, and recommend the most appropriate treatment plan for your specific needs.
Seeking Professional Medical Care
If you suspect that you have Inflammatory Bowel Disease or have already been diagnosed, it is crucial to seek professional medical care. A gastroenterologist, a specialist in digestive disorders, can provide an accurate diagnosis and recommend the most appropriate treatment plan for your specific condition.
It is important to establish a strong doctor-patient relationship and communicate openly about your symptoms, concerns, and treatment goals. Your healthcare provider may order various tests, such as blood work, stool samples, endoscopy, or imaging studies, to gather more information about the extent and severity of your disease. Based on these results, they can tailor a treatment plan that suits your needs.
Medication and Treatment Options for Inflammatory Bowel Disease
Medication plays a significant role in managing Inflammatory Bowel Disease. In collaboration with your healthcare provider, you may be prescribed various medications such as anti-inflammatory drugs, immunomodulators, corticosteroids, and biologics. These medications work by reducing inflammation, suppressing the immune system, or targeting specific molecules involved in the inflammatory process.
It is important to take these medications as directed by your healthcare provider and to inform them of any side effects or concerns. Some medications may take time to reach their full effect, so it is essential to be patient and consistent with your treatment. Regular follow-up appointments with your healthcare provider are necessary to monitor your progress, adjust medications if needed, and address any new symptoms or concerns.
In addition to medication, some individuals may require surgical intervention to manage their Inflammatory Bowel Disease. Surgery can involve the removal of damaged or inflamed sections of the digestive tract, aiming to alleviate symptoms and improve overall well-being. Surgical options vary depending on the specific condition and extent of disease involvement, and your healthcare provider will discuss the potential benefits and risks of surgery with you.
Adopting a Healthy Diet
Dietary modifications can greatly impact the management of Inflammatory Bowel Disease. While there is no one-size-fits-all diet for everyone with IBD, certain foods may trigger symptoms or exacerbate inflammation. It can be helpful to keep a food diary to identify any patterns between your diet and symptom flare-ups.
Some general dietary recommendations for individuals with Inflammatory Bowel Disease include:
- Avoiding spicy and greasy foods that may irritate the digestive tract. These foods can potentially trigger symptoms such as abdominal pain and diarrhea.
- Limiting the consumption of high-fiber foods, as they can be difficult to digest and may worsen symptoms. Instead, focus on incorporating easily digestible foods such as cooked vegetables, lean proteins, and low-fiber grains.
- Staying hydrated by drinking plenty of fluids, especially water. This helps maintain proper hydration and supports overall digestive health.
- Discussing dietary changes with a registered dietitian who specializes in gastrointestinal disorders. They can provide personalized guidance and help you create a well-balanced meal plan that meets your nutritional needs while managing your symptoms.
Managing Stress/ Inflammatory Bowel Disease
Stress and anxiety can worsen symptoms of Inflammatory Bowel Disease, so it is crucial to prioritize stress management techniques. Consider incorporating the following strategies into your daily routine:
- Engaging in regular exercise, such as yoga or walking, to promote relaxation and reduce stress. Physical activity releases endorphins, which are natural mood boosters.
- Practicing mindfulness and meditation to calm the mind and alleviate anxiety. Deep breathing exercises and guided imagery can be beneficial in reducing stress levels.
- Seeking support from friends, family, or support groups who understand the challenges of living with IBD. Sharing your experiences and feelings with others who can relate can provide emotional relief and a sense of belonging.
- Exploring stress-reducing activities such as art therapy, journaling, or listening to calming music. Find activities that you enjoy and that help you relax, allowing your mind and body to unwind.
Prioritizing Self-Care
Living with Inflammatory Bowel Disease can be physically and emotionally challenging. It is important to prioritize self-care to maintain overall well-being. Here are some self-care tips:
- Getting enough sleep to promote healing and reduce fatigue. Aim for a consistent sleep schedule and create a relaxing bedtime routine.
- Avoiding smoking and excessive alcohol consumption, as they can worsen symptoms and contribute to disease progression.
- Taking time for hobbies and activities that bring joy and relaxation. Engaging in activities that you enjoy can provide a much-needed distraction from the challenges of managing a chronic illness.
- Practicing good hygiene to prevent infections and complications. Wash your hands regularly and maintain a clean environment to reduce the risk of infections.
- Regularly scheduling medical check-ups and follow-ups with your healthcare provider. Staying proactive about your health and addressing any concerns promptly can help prevent complications and maintain disease control.
Seeking Emotional Support
The emotional toll of Inflammatory Bowel Disease should not be underestimated. It can be helpful to seek emotional support from professional therapists, counselors, or psychologists who specialize in chronic illness. They can provide coping strategies, help process emotions, and offer a safe space to discuss the challenges associated with IBD.
Support groups for individuals with Inflammatory Bowel Disease can also be valuable. Connecting with others who share similar experiences can provide a sense of community, validation, and encouragement. These groups can be found locally or online, allowing for ongoing support and shared knowledge
Coping with Inflammatory Bowel Disease requires a multi-faceted approach that encompasses medical care, lifestyle modifications, and emotional support. By working closely with healthcare professionals, adopting a healthy diet, managing stress, prioritizing self-care, and seeking emotional support, individuals with IBD can improve their quality of life and effectively manage their symptoms. Remember, every individual’s experience with IBD is unique, so it is essential to find coping strategies that work best for you.
VII. Complications and Long-Term Outlook of IBD
Inflammatory Bowel Disease (IBD) refers to a group of chronic inflammatory conditions that affect the gastrointestinal tract. The two main forms of IBD are Crohn’s disease and ulcerative colitis. Although these conditions can significantly impact a person’s quality of life, understanding the potential complications and long-term outlook of IBD is essential for effective management and patient support.
Complications of Inflammatory Bowel Disease
Intestinal strictures
Over time, inflammation in the digestive tract caused by IBD can lead to the development of scar tissue. This scar tissue can result in strictures or narrowings of the intestine, causing blockages and difficulties in the passage of stool. Intestinal strictures may lead to symptoms such as abdominal pain, bloating, and constipation. In severe cases, it may require surgical intervention to remove the strictures and restore normal bowel function.
Possible treatments and management for intestinal strictures include:
- Medications: Anti-inflammatory drugs, such as corticosteroids or immunomodulators, may help reduce inflammation and prevent further narrowing of the intestine.
- Balloon dilation: This procedure involves inserting a deflated balloon into the narrowed area of the intestine and inflating it to widen the passage.
- Surgical intervention: In cases where strictures are severe or recurrent, surgery may be necessary to remove the affected portion of the intestine and reconnect the healthy segments. In some cases, a temporary or permanent stoma may be created to divert the stool.
Fistulas
In some cases, the inflammation can extend through the intestinal wall, creating abnormal connections between different parts of the digestive tract or even with adjacent organs. These connections are known as fistulas and can cause pain, infection, and other complications. Fistulas may lead to symptoms such as persistent diarrhea, abdominal pain, and fever. Treatment options for fistulas depend on their location, severity, and associated complications.
Possible treatments and management for fistulas include:
- Medications: Antibiotics may be prescribed to treat or prevent infection associated with fistulas. Immunosuppressive medications, such as biologic therapies, may also be used to reduce inflammation and promote healing.
- Surgical intervention: In cases where fistulas do not heal with medications or cause severe symptoms, surgery may be necessary. Surgical options include removing the fistula tract, repairing or resecting the affected intestine, or creating a temporary or permanent stoma to divert the stool.
Abscesses
Pockets of pus can develop within the digestive tract due to ongoing inflammation. These abscesses can lead to infection, severe pain, and potentially require drainage or surgical intervention. Abscesses may cause symptoms such as fever, abdominal tenderness, and persistent pain.
Possible treatments and management for abscesses include:
- Drainage procedures: In many cases, abscesses can be drained using image-guided techniques, such as ultrasound or CT scan, to guide the placement of a drainage catheter. This helps to relieve symptoms and promote healing.
- Antibiotics: To treat or prevent infection associated with abscesses, antibiotics may be prescribed.
- Surgical intervention: In cases where abscesses are large, complex, or recurrent, surgery may be necessary to remove the abscess and repair any associated complications.
Perforations
In rare instances, severe inflammation can weaken the intestinal wall, leading to perforations or small holes. This condition is considered a medical emergency and requires immediate medical attention. Perforations may cause symptoms such as severe abdominal pain, fever, and signs of systemic infection.
Possible treatments and management for perforations include:
- Surgery: Emergency surgery is usually required to repair the perforation and remove any infected or damaged tissue. The surgeon may also perform a temporary or permanent colostomy or ileostomy to divert the stool and allow the affected area to heal.
Malnutrition and nutrient deficiencies
Chronic inflammation in the digestive tract can impair nutrient absorption, resulting in malnutrition and deficiencies in essential vitamins and minerals. This can further contribute to fatigue, weakness, and other complications. Malnutrition and nutrient deficiencies may lead to symptoms such as weight loss, anemia, and muscle wasting.
Possible treatments and management for malnutrition and nutrient deficiencies include:
- Nutritional therapy: A registered dietitian can help develop a personalized nutritional plan that focuses on optimizing nutrient intake and addressing deficiencies. This may involve dietary modifications, oral nutritional supplements, or, in severe cases, enteral or parenteral nutrition.
- Vitamin and mineral supplementation: Depending on the specific deficiencies, supplements may be prescribed to address nutrient imbalances.
- Regular monitoring: Regular blood tests and nutritional assessments can help identify and address any ongoing deficiencies or imbalances.
Colon cancer
Individuals with long-standing ulcerative colitis have an increased risk of developing colon cancer. Regular colonoscopies and surveillance are crucial to detecting precancerous changes or early signs of cancer in these patients. The frequency of colonoscopy surveillance depends on the duration and extent of the disease and the presence of any risk factors.
Possible approaches for colon cancer surveillance in individuals with ulcerative colitis include:
- Colonoscopy: This procedure allows for the direct visualization of the colon and the detection of any abnormal growths or changes. Biopsies may be taken during the procedure to evaluate suspicious areas.
- Chromoendoscopy: This technique involves using special dyes or stains during colonoscopy to enhance the detection of abnormal areas in the colon.
- Virtual colonoscopy: This non-invasive imaging technique uses CT scans to create detailed images of the colon, allowing for the detection of polyps or tumors.
Extraintestinal manifestations
IBD can also affect other parts of the body, leading to a variety of extraintestinal manifestations. These can include joint pain, skin rashes, eye inflammation, liver diseases, and osteoporosis, among others. The presence and severity of extraintestinal manifestations may vary among individuals and can significantly impact their quality of life.
Possible treatments and management for extraintestinal manifestations include:
- Medications: Depending on the specific manifestation, medications such as corticosteroids, immunomodulators, or targeted therapies may be prescribed to reduce inflammation and manage symptoms.
- Collaborative care: Individuals with extraintestinal manifestations may require the involvement of various healthcare professionals, such as rheumatologists, dermatologists, or ophthalmologists, to provide specialized care and treatment.
- Supportive measures: In addition to medical treatments, lifestyle modifications such as exercise, physical therapy, and the use of supportive devices may help manage symptoms and improve overall well-being.
Long-Term Outlook
While IBD is a chronic condition, it is important to note that the long-term outlook can vary significantly among individuals. Factors that influence the disease course and prognosis include the type of IBD, disease severity, response to treatment, and individual patient characteristics.
Disease remission
With appropriate medical management and lifestyle modifications, many individuals with IBD can achieve periods of remission where their symptoms are minimal or absent. These remission periods can vary in duration and provide relief from the active disease. Achieving and maintaining remission is the primary goal of treatment for IBD.
Flare-ups and relapses
IBD is characterized by periods of active disease and periods of remission. Flare-ups or relapses can occur unpredictably, causing a recurrence of symptoms. It is important for individuals with IBD to work closely with their healthcare team to identify triggers and manage flare-ups effectively. Early recognition and prompt treatment of flare-ups can help minimize their impact on daily life and prevent complications.
Medical treatments
Various medications are available to control inflammation, alleviate symptoms, and maintain remission in individuals with IBD. These include aminosalicylates, corticosteroids, immunomodulators, biologic therapies, and targeted therapies. The choice of treatment depends on disease severity, location, and individual patient factors. Regular monitoring and adjustments to the treatment plan may be necessary to optimize outcomes and minimize side effects.
Surgical interventions
In some cases, surgery may be necessary to manage complications or improve quality of life. Surgical options for IBD include bowel resection, strictureplasty, colectomy, and ileostomy or colostomy procedures. Surgery can help alleviate symptoms, but it is not a cure for IBD. The decision to undergo surgery is typically made in collaboration with the healthcare team, taking into account factors such as disease severity, response to medical therapy, and individual patient preferences.
Psychological impact
Living with a chronic condition like IBD can have a significant psychological impact on individuals. Anxiety, depression, and reduced quality of life are common among patients. Adequate emotional support, counseling, and involvement of mental health professionals can help individuals cope with the challenges posed by IBD. It is important to address both the physical and emotional aspects of the disease to improve overall well-being and treatment outcomes.
Lifestyle modifications
Adopting a healthy lifestyle can have a positive impact on managing IBD. This includes following a nutritious diet, avoiding trigger foods, staying physically active, managing stress levels, getting adequate sleep, and avoiding tobacco and excessive alcohol consumption. A registered dietitian can provide guidance on specific dietary modifications that may help reduce symptoms and promote overall health.
Patient support and education
Access to support groups, patient education programs, and resources can empower individuals with IBD to actively participate in their own care. Understanding the disease, treatment options, and self-management strategies can improve long-term outcomes and overall well-being. Support groups and online communities provide an opportunity to connect with others who are facing similar challenges, and educational resources offer valuable information and guidance.
In conclusion, while IBD can present various complications and challenges, with appropriate medical management, lifestyle modifications, and support, individuals living with IBD can achieve and maintain remission, effectively manage flare-ups, and lead fulfilling lives. Regular monitoring, close collaboration with healthcare professionals, and staying informed about the latest advancements in IBD treatment are key to ensuring the best possible long-term outlook for patients with IBD.
FAQ About Inflammatory Bowel Disease
1. What are the primary symptoms of Inflammatory Bowel Disease?
- Abdominal pain and cramping
- Diarrhea
- Rectal bleeding
- Weight loss and malnutrition
2. How can I manage abdominal pain and cramping associated with Inflammatory Bowel Disease?
- Taking prescribed medications such as anti-inflammatory drugs, pain relievers, or antispasmodics
- Applying heat to the abdomen or taking warm baths
- Practicing stress-reducing techniques like deep breathing, meditation, or yoga
3. What can I do to manage diarrhea caused by Inflammatory Bowel Disease?
- Stay hydrated by drinking plenty of fluids
- Avoid foods that can exacerbate diarrhea, such as spicy or greasy foods, caffeine, and alcohol
- Incorporate fiber-rich foods gradually into the diet, but consult with a healthcare professional or registered dietitian for personalized recommendations
4. How can I address weight loss and malnutrition associated with Inflammatory Bowel Disease?
- Work with a registered dietitian to develop an individualized meal plan
- Incorporate nutrient-dense foods into the diet
- Consider nutritional supplements or enteral nutrition (tube feeding) if recommended by a healthcare professional
5. What are the two primary types of Inflammatory Bowel Disease (IBD)?
- The two primary types of Inflammatory Bowel Disease (IBD) are Crohn’s disease and Ulcerative Colitis.
6. What are the common symptoms of Crohn’s disease?
- Common symptoms of Crohn’s disease include abdominal pain, diarrhea, weight loss, and malnutrition.
7. What are the common symptoms of Ulcerative Colitis?
- Common symptoms of Ulcerative Colitis include abdominal pain, bloody diarrhea, and a constant urge to defecate.
8. What are the possible causes and risk factors for developing IBD?
- The possible causes and risk factors for developing IBD include genetic factors, environmental triggers, immune system dysfunction, and microbiome imbalance.
The article provided is for informational purposes only and should not be considered as medical advice. It is always recommended to consult with a qualified healthcare professional for diagnosis and treatment of any medical conditions.